
Internal hemorrhoids are further classified depending upon the severity of the prolapse.

They are covered by columnar epithelium, innervated by visceral nerve fibers and are not painful. Internal hemorrhoids (IH) are derived from the endoderm. Hemorrhoids are classified as internal or external, depending upon their location proximal or distal to the dentate line, respectively. These figures may be an underestimation of the actual disease burden, as a substantial percentage of patients suffering from HD may not report it to a physician besides, many patients suffering from HD have minimal symptoms and may not seek medical help. Approximately 4.4 to 36.4% of the general population may be affected by HD. The prevalence reported in literature varies. Hemorrhoidal disease (HD) is one of the most common ano-rectal disorders and ranks amongst the most frequent reasons of visit to any outpatient surgical facility.
There were no wound related complications.Ĭonclusion Stapled hemorrhoidectomy can be performed easily and offers good results in patients with recurrent HD.Ĭircular anal dilator repeat stapled hemorrhoidectomy Patients with recurrent HD had severe pain scores with SH as compared to patients who underwent SH at the first time. There were no adverse events related to the technique. Results Stapled hemorrhoidectomy (SD) was performed in 13 patients who had history of previous surgical intervention for HD. A mean follow-up of 22 months was achieved. A modification of the standard technique was adopted for patients with recurrent HD. Thirteen out of 87 patients (15%) had history of previous intervention for HD.
#Stapled hemorrhoidopexy complications series
Material and Methods The present prospective case series enrolled a total of 87 patients (54 male/33 female). The ideal way to deal with recurrent HD is not clear. Postsurgical symptomatic recurrence rates are low and vary between different techniques. Every surgical option has its own indications and limitations. The treatment modalities can be surgical or nonsurgical. 10.Overview Hemorrhoidal disease (HD) is a common surgical disorder. Stapled transanal rectal mucosectomy ten years after. A prospective evaluation of stapled haemorrhoidopexy/rectal mucosectomy in the management of 3rd and 4th degree haemorrhoids. Slawik S, Kenefick N, Greenslade GL, Dixon AR. In: Proceedings of the 6th World Congress of Endoscopic Surgery. Treatment of haemorrhoidal disease by reduction of mucosal and haemorrhoidal prolapse with circular-suturing device: a new procedure. Chirurgia colonproctologica e pelvi perineale.
#Stapled hemorrhoidopexy complications full
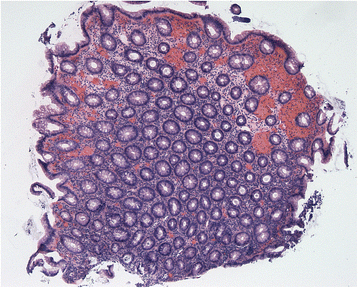
This concept defines the entity of the surgical procedure and excludes a direct correlation with an increased rate of complications.Ĭomplications full thickness histopathology rectal mucosectomy stapled hemorrhoidopexy.Ĭopyright © 2021 Eberspacher, Magliocca, Pontone, Mascagni, Fralleone, Gallo and Mascagni. Discussion: Stapled hemorrhoidopexy is not a simple mucosectomy but a resection of the rectal wall with almost all its layers. No statistically significant difference in the rate of complications was found when stratifying patients according to the thickness of the resection. Results: Of the 137 histological slides available, 13 were only mucosectomies (9.5%), and 124 presented also the submucosa and muscularis propria (90.5%)-50/58 patients in Group A, 28/28 in Group B, and 46/51 in Group C. For every specimen, we reconstructed the history of the corresponding patient and the incidence of complications. We evaluated the actual wall layers included in the stapled rectal ring. Patients were divided into three groups, according to the stapler used: Group A (single PPH®), Group B (double PPH®), and Group C (CPH34 HV™). Materials and Methods: We histopathologically analyzed surgical samples from patients who underwent stapled hemorrhoidopexy performed between 20. The aims of our retrospective, single-center study were to demonstrate if the excised specimen comprises only the mucosa or more wall rectal layers and if the latter excision should be considered a technical mistake with an increase in complications. Introduction: Stapled hemorrhoidopexy was originally defined as a rectal mucosectomy.


 0 kommentar(er)
0 kommentar(er)
